The ERC Guidelines 2021: Post-resuscitation care (Part 6/7)
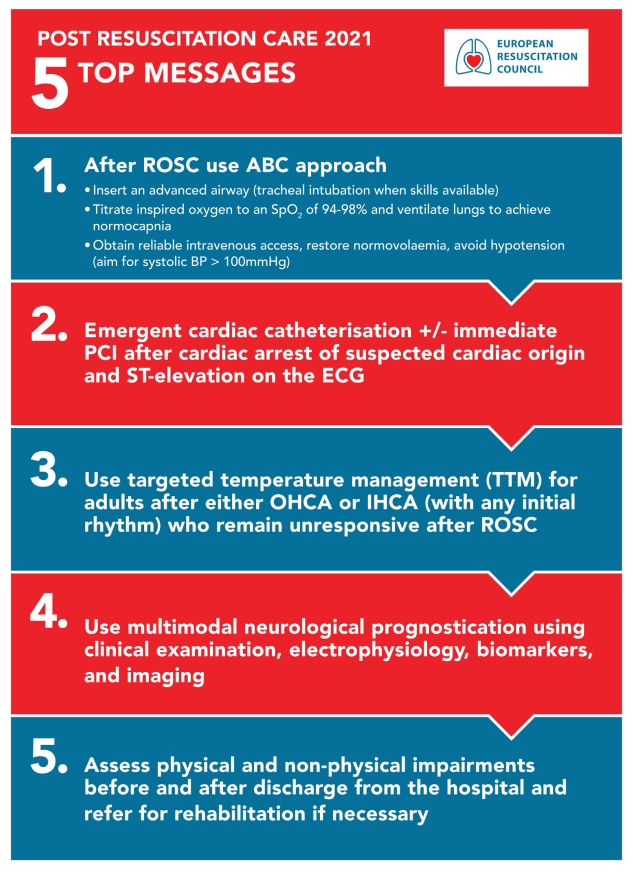
The ERC 2021 guidelines on post-resuscitation care contain major updates to the 2015 version on coronary angiography, blood pressure target, seizure treatment, temperature control, and other topics.
Eight guideline areas have undergone major updates since 2015
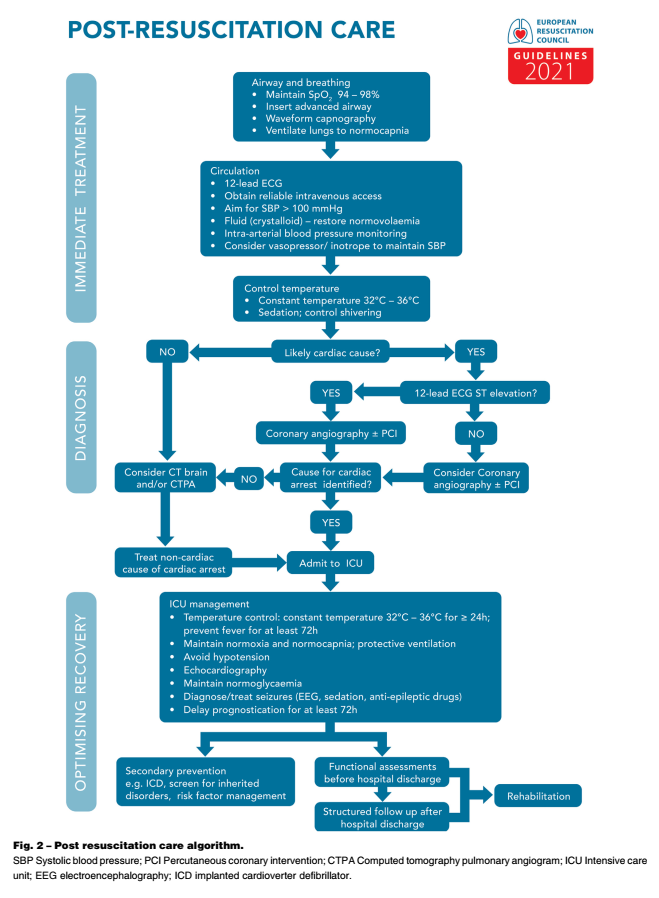
The ERC 2021 Guidelines on post-resuscitation care contain an extensive update from the 2015 version. Topics covered in the 2021 update include post-cardiac arrest syndrome, diagnosis of causes of arrest, oxygenation and ventilation, coronary reperfusion, haemodynamic monitoring and management, control of seizures, temperature control, general intensive care management, prognostication, long-term outcome, rehabilitation, and organ donation.
Made in cooperation with our partners from esanum.it
In 2015, the European Resuscitation Council (ERC) and the European Society of Intensive Care Medicine (ESICM) collaborated to produce their first joint guidelines for post-resuscitation care, which were co-published in the journal Resuscitation and Intensive Care Medicine. The most important innovations in the ERC 2021 Guidelines for post-resuscitation care include:
-
Coronary angiography: In patients with ROSC after OHCA without ST-segment elevation on ECG, urgent cardiac catheterisation laboratory evaluation should be considered if there is a high estimated probability of acute coronary occlusion (e.g. patients with haemodynamic and/or electrical instability).
-
Blood pressure target: Avoid hypotension (<65 mmHg) + achieve a mean arterial pressure such that adequate urine output is obtained (>0.5 ml kg-1 h-1) and normal or decreasing lactate.
-
Treatment of seizures: For convulsions after cardiac arrest, levetiracetam or sodium valproate are suggested as first-line antiepileptics, in addition to sedative drugs.
-
Temperature control: TTM (target temperature management) is recommended for adults after OHCA or IHCA (with any initial rhythm) who remain unresponsive after ROSC + maintain target temperature at a constant value between 32 °C and 36 °C for at least 24h + avoid fever (>37.7 C) for at least 72h after ROSC in patients who remain comatose.
-
General intensive care management post-ROSC:
- Use short-acting sedatives and opioids.
- Avoid routine use of curari in patients undergoing TTM, but may be considered if severe chills occur during TTM.
- Administer routine stress ulcer prophylaxis.
- Achieve a blood glucose of 7.8-10 mmol/l (140-180 mg/dl) using an insulin infusion if necessary; avoid hypoglycaemia (<4.0 mmol/l or <70 mg/dl).
- Start enteral nutrition at low doses (trophic) during TTM and increase after warming if indicated. If the target temperature of TTM is 36 °C, enteral nutrition dosages can be increased early during TTM.
- Routine use of antibiotic prophylaxis is not recommended.
-
Prognostication: In a comatose patient with M ≤3 at ≥72h after ROSC, in the absence of confounding factors, an unsatisfactory outcome is likely when two or more of the following predictors are present: absence of pupillary and corneal reflexes at ≥72h, bilaterally absent N20 SSEP wave at >24h, highly malignant EEG at >24h, NSE >60 mg/l at 48 h and/or 72h, myoclonus ≤72h, or diffuse and extensive anoxic brain injury seen by CT/MRI.
- Rehabilitation: eseguire valutazioni funzionali dei danni fisici e cognitivi/psicologici prima della dimissione dall'ospedale per identificare le prime esigenze di riabilitazione precoce e indirizzare alla riabilitazione se necessario + organizzare il follow-up per tutti i sopravvissuti all'arresto cardiaco entro 3 mesi dalla dimissione dall'ospedale, tra cui: screening per problemi cognitivi, screening dei problemi emotivi e dell'affaticamento, supporto ai sopravvissuti e ai membri della famiglia.
Always post-ROSC
- SpO2 94-98%
- Systolic blood pressure >100 mmHg
- Capnography
- 12-lead ECG
- Blood pressure measurement
- Temperature management
Diagnostics in the emergency department according to ROSC
- Highly probable cardiac aetiology + ST-segment elevation: emergency coronarography.
- Highly probable cardiac aetiology without ST-segment elevation: consider emergency coronarography.
- Unlikely cardiac genesis: consider CCT +/- CT chest (pulmonary embolism?).
The ERC 2021 Guidelines present a major update on cardiopulmonary resuscitation and provide the most up-to-date evidence-based procedures for citizens (lay professionals), healthcare professionals and health policy makers across Europe. The ERC Guidelines 2021 can be downloaded here: New ERC Guidelines.
An overview of the most important ECR Guidelines 2021 changes is available in this esanum article series:
- The ERC Guidelines 2021 (Part 1/7)
- Main Changes (Part 2/7)
- Adult Advanced Life Support (ALS) (Part 3/7)
- Peri-Arrest Arrhythmias (Part 4/7)
- Cardiac Arrest in Special Circumstances (Part 5/7)
- Post-Resuscitation Care (Part 6/7)
- Resuscitation in Children (Part 7/7)
Sources:
1. Nolan JP, Sandroni C, Böttiger BW, Cariou A, Cronberg T, Friberg H, Genbrugge C, Haywood K, Lilja G, Moulaert VRM, Nikolaou N, Mariero Olasveengen T, Skrifvars MB, Taccone F, Soar J. European Resuscitation Council and European Society of Intensive Care Medicine Guidelines 2021: Post-resuscitation care. Resuscitation. 2021 Apr;161:220-269. doi: 10.1016/j.resuscitation.2021.02.012. Epub 2021 Mar 24. PMID: 33773827.
2. Fandler M. Neue Reanimationsleitlinien 2021 (ERC) Zusammenfassung. Nerdfallmedizin.de. 25/03/2021