Medical History: John Snow, a map, and a pump
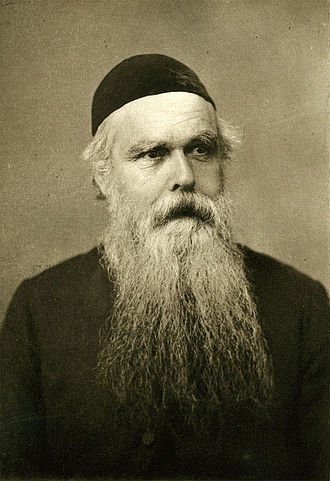
The bacillus "Vibrio cholerae", isolated 30 years before Koch by the Italian physician Filippo Pacini, is quite the menace. An agent of cholera, its brutal bacterial infection has sent millions of homo sapiens to the grave.
The bacillus "Vibrio cholerae", isolated 30 years before Koch by the Italian physician Filippo Pacini, is quite the menace. An agent of cholera, its brutal bacterial infection has sent millions of homo sapiens to the grave.
Made in cooperation with our partners from esanum.fr
In the long fight against a disease that is exclusively human and still endemic in many parts of the world, one name stands out: that of John Snow. This is not related to the “Game of Thrones” character. But instead, this story is about an English physician whose intuition played a decisive role in understanding cholera. Let's go back in time to mid-19th century London.
One of the side effects of great pandemics is their ability to enrich vocabulary. Cholera is no exception: in France, the expression “avoir une peur bleue” (literally meaning “to be scared blue”), has its English equivalent in “to be scared to death”. This expression was a direct reference to the particularly spectacular blue tones that marked the faces of the sick, a few hours or minutes before death.
This illness has left its mark on several generations and has made its way into the works of writers such as Thomas Mann1, Jean Giono2, or Gabriel Garcia Marquez3. Able to kill a patient in a few hours, with a case-fatality rate that reached 60 to 70% in the 19th century, cholera is characterized first and foremost by its suddenness: "in less than 24 hours," wrote French infectious disease specialist Marc Gentilini, cholera makes a victim "resemble a deportee leaving a famine camp"4.
Silent and deadly
Leaving a friend in good shape one evening, finding them dead the next day without any warning signs: this reality, described a thousand times, traumatic for those around the lost loved one, shows that cholera strikes quickly and silently. Beyond the trauma evoked by countless letters, articles, and diaries from the 18th century onwards, it is difficult to find a more clinical and frightening description than that of a Belgian physician, Dr. Tilman, when the epidemic hit the town of Virton in the Belgian Ardennes.
In 1849, he wrote: "the invasion (...) took place around two or three in the morning (...) under the appearance of indigestion. Vomiting of whitish liquid was followed by stools of the same nature. When the condition was severe, the pulse rate would soon slow down, the eyes would sink deeper and deeper into the eye sockets, the body's heat would decrease, the skin would turn cyanotic, and a general and unbearable uneasiness would manifest itself. The cramps in the arms and legs tortured the patient."
An intestinal disease, cholera results in sudden and acute dehydration, capable of causing a loss of 10 to 15% of the total weight in a few hours without the possibility to compensate for the water loss due to the vomiting that affects the patient. "A burning thirst devoured him, the pulse stopped beating, the urine was suppressed, and if the disease was not tamed, the body was covered with a cold, viscous sweat, breathing slowed down, the voice weakened and life often ended without agony. However, the patient maintained the presence of mind until the last moment, and sometimes, when he was not tormented by cramps and vomiting, he seemed to see the end of his life calmly and without anxiety", detailed Dr. Tilman.
Soho, 1854
Dr. Tilman wrote these lines in 1849, three years after the start of the third major cholera pandemic out of the seven that have been recorded in modern times5. Originating in the Asian region, the bacillus transited through the Maghreb before arriving in Europe, boosted by the extensive colonial trade taking place across regions at the time. The "comma bacterium" - to use the nickname given by the German bacteriologist Robert Koch in reference to its characteristic curved shape - spread throughout Europe.
In London, during the summer of 1854, the epidemic saw a particularly brutal outbreak in the middle of London's West End's Soho district, right in the heart of the city. Other outbreaks had already been detected in the British capital, but on 31 August 1854, 127 people died in Broad Street (now called Broadwick Street) in three days. The ensuing panic led to the flight of three-quarters of the district's inhabitants and to a fear that spread all the more rapidly throughout the city as, despite these departures, the epidemic continued unabated: by 10 September, the threshold of 500 dead was crossed.
Faced with the epidemic, political and health officials were struggling to propose an effective response, for the sole reason that several theories of contagion were still clashing, including the good old theory of miasmas - that is "bad air"6, which was still considered by many as the most credible, that is, in the absence of a theory of germs that would only become established twenty to thirty years later.
And there was indeed no shortage of this vicious, unhealthy air in Soho. Like the whole capital, the district had seen its population explode without basic public services to follow suit. Sanitation facilities were non-existent, the streets barely paved, and no sewers had been built under the West End. The craftsmen and traders of the area - including stables, butchers, and slaughterhouses - let the weather "rinse" much of the blood and excrement that their activity brought with it, throwing the rest directly into a river Thames that had never been so dirty.
The man who was going to play a decisive role in this situation was a physician who set up his general practice right in the neighborhood, at 54 Frith Street: John Snow.
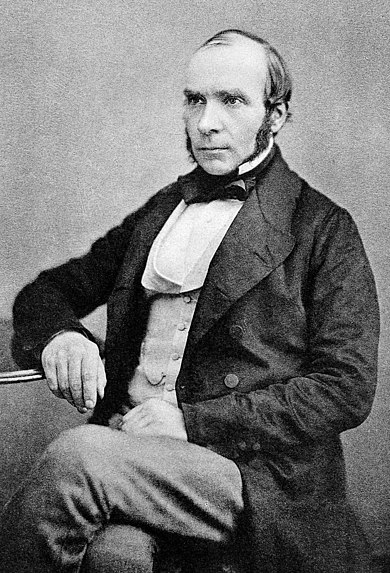
A physician of the poor at a time when many of his colleagues were looking for a "posher" clientele in less populous neighborhoods, Snow had a front-row seat to witness the ravages of the epidemic that struck Soho at the very end of August 1854.
The sanitary drama, however, provided an opportunity to verify one of his old intuitions. John Snow did not believe in the miasmas theory and his doubts only grew stronger when he observed that the artisans deemed responsible for the spread of the disease (such as butchers) were not the first to be affected by cholera. After a few autopsies, he noted that cholera did not affect the lungs but the intestines of the patients - curious, for a disease one is supposed to catch by breathing unhealthy air. If air is not the vector, how is the disease transmitted? Snow placed his bet on the area's drinking water. Or, given the salubrity levels at the time, at least it was the water drunk by locals.
He then conducted a thorough investigation in the neighborhood with the help of the local reverend, Henry Whitehead.
Snow took a series of samples from the neighborhood pumps. Keep in mind, there was still no pipe system distributing water into each individual flat. But Snow did not spot anything special under the microscope.
The world's simplest sanitary answer
Not discouraged, he then had a brilliant idea: to locate on a Soho map the precise place where the affected patients lived. By crossing this early geolocation exercise with a scrupulous study of the patients' daily life, he noticed that they all shared a common habit: they all got their water from a pump located in Broad Street. Better still, he discovers that the only victim who did not live in this area had lived there before and had kept the habit of coming to fill her bucket at the famous pump, a diversion that the patient justified by the "good taste" of the water obtained at that pump.
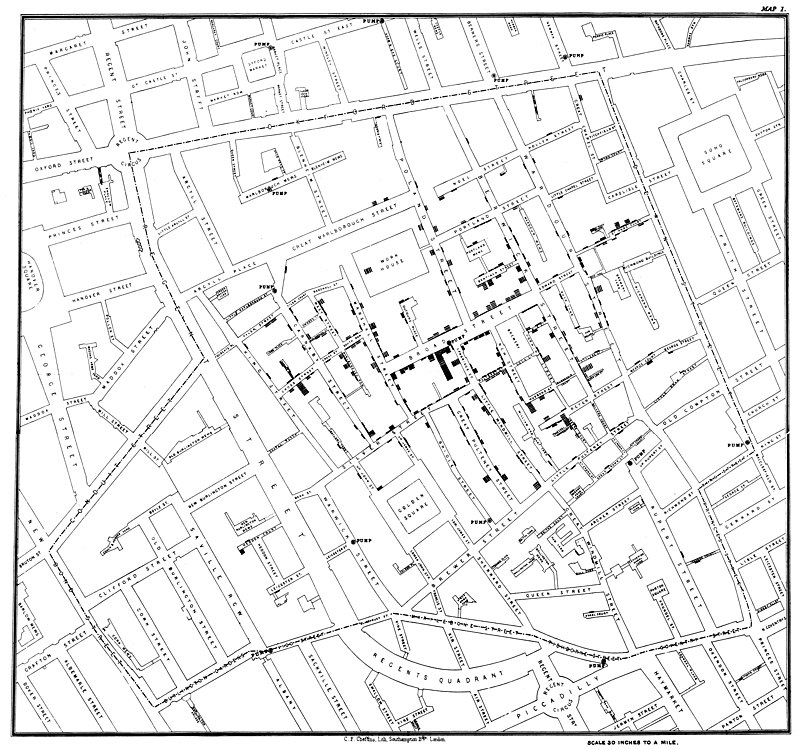

Zooming in to the very source of an outbreak, John Snow style.
Based on the weight of his findings, John Snow posed to the authorities one of the most simple questions in the history of prophylaxis: do you take the handle off the pump?
Patient zero
The results were immediate. The epidemic was stopped, after having caused the death of 616 Londoners in ten days. But there were questions still lingering the issue, given that John Snow, being a man of integrity, was the first to admit that the contaminations had already begun to slow down before the pump handle was removed.
Cholera is transmitted through water, and Snow was convinced of this. But, by what, in the water? With the help of Reverend Henry Whitehead, Snow digs and digs deeper into his survey at the site in question. And he discovers a notable fact: the epidemic of the summer of 1854 really started a few days after the death of a very young child, the first to be affected. Following the trail of his patient zero, Snow observed that the boy's mother was washing his nappies and getting rid of the water by pouring it from her bucket into a pit a few yards from the Broad Street well.
Snow did his research, and bingo: he discovered that the pit was communicating with the well. Going even further, Snow compares the Soho epidemic with cholera cases in other neighborhoods. And he goes even further: he finds that the number of patients affected is higher where water samples are more likely to be contaminated by rubbish and other refuse.
Unlike the London water of the time, Snow arrives at a clear hypothesis. Cholera is transmitted by drinking water contaminated by fecal matter, a hypothesis that he states publicly in an 1855 book. Except that...
Except that his theory, which has been definitively confirmed since then, ran up against a wall of skepticism in the academic community. But perhaps a cultural bias for this reaction could not be ruled out. After all, the idea of oral contamination by fecal matter was something that offended the puritan minds of Victorian society. Also, Snow was perhaps the victim of a certain form of jealousy from colleagues, many of them directing ad personam attacks against him, on the ground that Snow was not an epidemiologist.
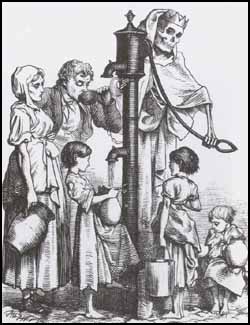
The French approach to the John Snow discovery: "I treat cholera with champagne, it's the Mayeux system" Anti-cholera cartoon (ed. Aubert - 1932)
Some even went as far as to belittle him as a "simple general practitioner", and more so, to point the fact that he was based in a working-class district - an attack all the more inappropriate as it was completely false. He was anything but unknown in the scientific community since he had invented an ether inhaler in 1849. His machine, which could precisely control the dosage of an anaesthetic7 made him one of the great voices in the nascent specialty of anesthesiology since Queen Victoria herself delivered her eighth child under anesthesia, taking advantage of Snow's invention.
Unfair and often misplaced, these attacks seriously slowed down awareness of a disease whose kinetics can be seriously reduced with a series of hygiene measures that are sometimes very simple, but which would only become more refined over the following decades since the London outbreak of 1854.
Notes :
1. Thomas Mann, Der Tod in Venedig / Death in Venice, 1912
2. Jean Giono, Le hussard sur le toit / The Horseman on the Roof, 1951
3. Gabriel García Márquez, El amor en los tiempos del cólera / Love in the Time of Cholera, 1985.
4. Marc Gentilini, Medecine Tropicale, , Flammarion, 1993.
5. The seventh outbreak is still going strong, with over 100,000 deaths a year.
6. This is the primary meaning of the Italian word malaria.
7. And he did not even file a patent for the device, in order to allow the medical community to use it as massively as possible.