Therapy and progression:
Such sharply demarcated and densely grouped pustules allow the visual diagnosis of herpes progenitalis. The medical history and the residual lesions indicate that recurrences are quite frequent. The extensive reddening, however, speaks in favour of a secondary bacterial superinfection in the sense of a gluteal erysipelas. This in turn was the result of mechanical irritation due to the hours of sitting required for work and scratching due to itching. The point of entry was then the herpes-related barrier defect. The predominantly viral infection leads to a depletion of the white blood count, which explains the leftward shift in the blood count that is to be expected for erysipelas, and which is absent here. Finally, microbiology was also able to prove the HSV infection. The Candida detection corresponded to non-specific colonisation. In the case of erysipelas, no specific pathogen detection from the smear was to be expected.
Herpes progenitalis: The first infection is severe and painful
Herpes progenitalis corresponds to the secondary manifestation of genital herpes, the genital primary infection of which is inapparent in the vast majority of cases. While the orofacial infection ("cold sores") is usually the result of a primary infection in childhood (almost complete infestation worldwide), the first infection of genital herpes usually only occurs after puberty and reaches an infestation rate of around 20-25% in adulthood. Genital herpes is a sexually transmitted disease (STD). Although HSV-2 is the leading pathogen in genital herpes, HSV-1 can also be the cause. The "girdle rule" (HSV-1 above, HSV-2 below the girdle) often quoted in dermatological lectures is therefore no longer reliable.
The initial genital infection is characterised by severe and painful blisters in the genital area, which may tend to ulcerate. This primarily affects the female genital mucosa in the form of vulvovaginitis herpetica (Figure 2) but also (albeit more rarely and milder) the glans and foreskin of the man as balanoposthitis herpetica. There is usually a severe feeling of illness with headaches, fever and swelling of the lymph nodes.

a

b
c

d
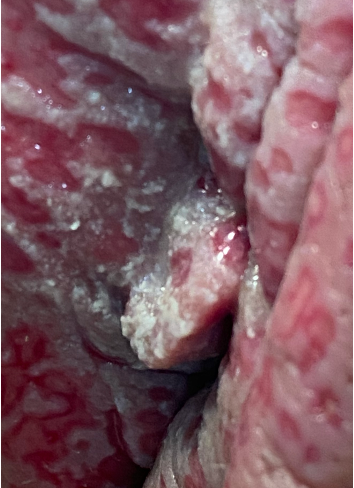
Fig. 2: Initial genital infection with HSV-2 in a 43-year-old female patient (a). Pronounced superficial mucosal ulceration of both the labia majora and the labia minora (b,c). Balanoposthitis herpetica in another patient (d).
In both orofacial and genital herpes, HSV is transmitted via direct contact with the mucous membranes (saliva, sexual contact). Herpes simplex viruses persist in the regional nerve ganglia for life after the initial infection. From this latency stage, HSV can be reactivated along the sensitive nerves of the skin. Trigger factors for reactivation are physical exertion, trauma, stress and menstruation.
The initial infection of orofacial herpes is gingivostomatitis herpetica, which in most cases is inapparent or mild. Reactivation then usually takes place in the oral or perioral facial area. Genital herpes affects the genital area (genital herpes), but much more frequently the gluteal area or the lower abdominal region (progenital herpes). Typical are the prodromal symptoms before the appearance of the grouped blisters the size of a grain of rice, which quickly transform into pustules and heal after 1 to 2 weeks. The subjective symptoms are usually mild, but severe pain is also possible.
The frequency of genital herpes recurrence caused by HSV-2 is five times higher than that caused by HSV-1. Symptoms occur more frequently in men. It should be noted that infected patients can excrete viruses despite the absence of symptoms. Women infected with genital herpes recidivans show asymptomatic virus excretion on up to 20% of all days, regardless of a current recurrence.
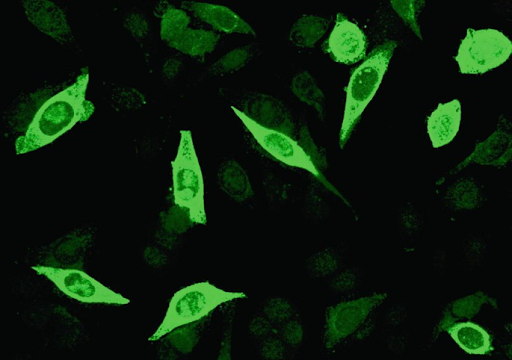
The lesional dry smear for PCR or immunofluorescence is the diagnostic method of choice. Antibody serology can provide information about the infection by detecting HSV-specific IgM or IgG antibodies (Figure 3).

a

b
c
Fig. 3: Lesional smear in herpes progenitalis both in the primary infection (a) and in the recurrent manifestation (b). Positive immunofluorescence in HSV infection (c).
It is not at all uncommon - and also in the present case - for progenital herpes to be misinterpreted as recurrent shingles. However, this would be much more painful, more clearly manifested in the dermatome and, in the case of immunocompetence, recurs after years at most. In many cases, the grouped pustules are also interpreted as impetigo contagiosa and then treated with antibiotics. The residual lesions in the present case may also be reminiscent of PVL-positive pyoderma. Panton-Valentine leucocidin (PVL)-producing Staphylococcus aureus (PVL-SA) strains are frequently associated with recurrent abscesses in otherwise healthy young people. These often affect the trunk, buttocks and proximal extremities. The exotoxin that causes progressive skin infections cannot be detected in the apparently sensitive antibiogram, but requires an explicitly formulated laboratory requirement and also special antibiotics.
In primary genital herpes, acute vaginal candidiasis is the most common misdiagnosis, although pain and swelling of the lymph nodes are the main symptoms of genital herpes. Of course, gram-positive or gram-negative pyoderma must also be differentiated.
In the present case, treatment with valaciclovir 2x500mg over 5 days was carried out. This treatment should be repeated at the onset of prodromal symptoms during each episode. The aim is to reduce the frequency of recurrences, as complete eradication of the pathogen is not possible.
Parallel to the antiviral therapy, antibiotic treatment with flucloxacillin 3x 0.75g p.o. for 7 days was administered due to the suspicion of secondary erysipelas. Both the erysipelas and the herpes progenitalis healed during treatment.
Conclusion: Reducing the frequency of genital herpes episodes through antiviral therapy
Genital herpes is an infection, usually with HSV-2, in the genital area and is an STD. The primary infection is usually inapparent. Recurrences often manifest as herpes progenitalis, which must be distinguished from zoster and pyoderma. Asymptomatic infected persons can also be contagious. Antiviral therapy can significantly reduce the frequency of recurrence. Due to the good therapeutic successes against AIDS, including post and pre-exposure prophylaxis, and the resulting increase in carelessness, a general increase in STDs has been observed.


