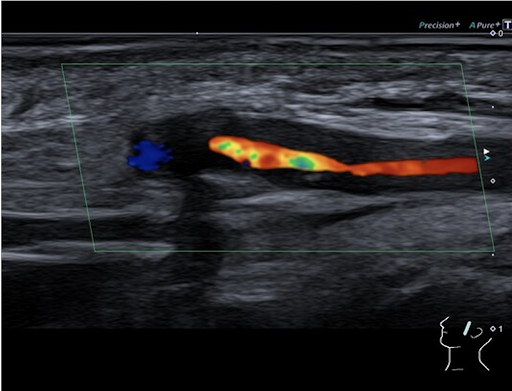
Diagnosis
Temporal arteritis (giant cell arteritis) in a patient with known polymyalgia rheumatica.
What is giant cell arteritis?
Giant cell arteritis (GCA) is "related" to another rheumatic disease, polymyalgia rheumatica (PMR). Both can occur independently but are often diagnosed together or overlap. The two diseases practically never occur before the age of 50, with the prevalence of PMR being approximately one to two per 1,000. Polymyalgia rheumatica typically manifests as severe muscle pain in the shoulder and pelvic girdle area, accompanied by significantly elevated inflammatory markers and general symptoms such as fatigue.
Approximately 10 to 20 percent of PMR patients also develop giant cell arteritis over time. Conversely, 40 to 60 percent of patients with giant cell arteritis exhibit typical polymyalgia symptoms. The characteristic signs of temporal arteritis that are particularly clinically significant include new-onset temporal headaches, pain when chewing, and visual disturbances such as blurred vision, sudden loss of vision, or occasionally double vision. Overall, 20 to 50 percent of patients with giant cell arteritis develop visual symptoms that require prompt diagnosis.
Treatment and Course of Disease
Following initial treatment with high-dose prednisolone (60 mg/day), the patient experienced significant improvement in headaches and visual disturbances within 48 hours. Inflammatory markers also gradually began to normalize. After two weeks of stable clinical course, the patient was discharged to outpatient care. She received a reduced prednisolone regimen with regular monitoring of inflammatory parameters and clinical symptoms. To minimize the risk of recurrence, maintenance treatment with prednisolone at a dose of 10 mg/day for a period of two years was recommended.