Therapy and progression:
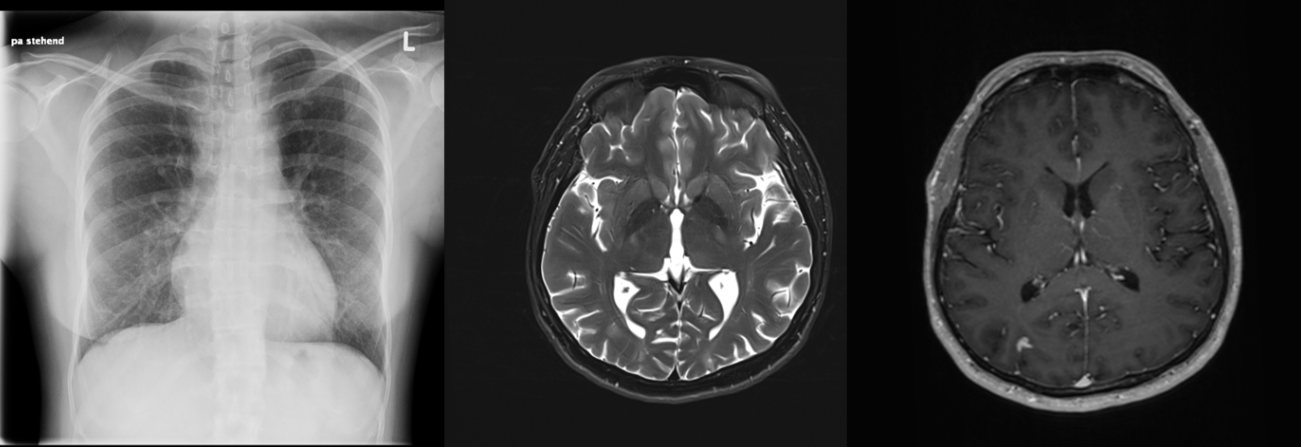
The infectious disease investigation initially showed a positive quantiferon test, followed by a positive tuberculosis PCR, and the detection of acid-fast rods in the bronchoalveolar lavage (BAL), leading to the diagnosis of open miliary tuberculosis. The cerebrospinal fluid (CSF) PCR was positive for tuberculosis in the lumbar puncture.
In addition, an immune status of multigrade lymphopenia was observed, which, after consultation with colleagues in immunology, was most likely to be assessed as reactive and, taking into account the pregnancy, as a decisive risk factor. A transesophageal echocardiography (TEE) was postponed in the case of infarctions that were initially discussed in terms of their morphological morphology, including septic embolism.
Due to the patient's compromised condition, a cesarean section was performed, and the patient gave birth to a healthy premature infant.
A four-fold anti-tubercular therapy with moxifloxacin, rifampicin, isoniazid (+vitamin B6) and pyrazinamide was started.
Postpartum, treatment with dexamethasone was started and later switched to prednisone. Cotrimoxazole was administered to prevent Pneumocystis jirovecii pneumonia. Tests for HIV, toxoplasmosis and other infectious and immunological differential diagnoses remained negative.
After two months, the patient was in a significantly better condition and could be discharged back home. After six months, the pneumonic consolidations and CNS lesions had clearly regressed.
Miliary tuberculosis, a rare but serious disease
Miliary tuberculosis is a serious form of tuberculosis characterised by the dissemination of mycobacterium tuberculosis bacteria to various organs of the body. This form of tuberculosis, which gets its name from the milium-like (millet-seed-sized) tubercles found in the affected organs, can be life-threatening if left untreated.
Epidemiologically, miliary tuberculosis is less common than other forms of tuberculosis, but is associated with a higher morbidity and mortality rate. It can occur in any age group, but has a higher incidence in children and in immunocompromised individuals, such as those with HIV infection. Globalisation and the increase in travel and migration have led to miliary tuberculosis cases occurring in countries with a low prevalence of tuberculosis.
The development of miliary tuberculosis
Reactivation of latent tuberculosis infection can also lead to the development of miliary tuberculosis, especially in individuals with weakened immune systems. In Ms S., the immunosuppression caused by pregnancy may have been a trigger.
Pathogenetically, miliary tuberculosis develops through the haematogenous spread of tuberculosis bacteria from a primary site of infection in the lungs or another organ. This dissemination can be favoured by a weakened immune system, which makes the disease particularly dangerous for people with existing immune deficiencies. The process leads to the formation of small, granulomatous lesions in various organs, including the lungs, liver, spleen and central nervous system.
Miliary tuberculosis: personalised treatment is necessary
The treatment of miliary tuberculosis usually involves a combination of several antibiotics over an extended period of time to eradicate the bacteria and avoid the development of resistance. Treatment can be complicated by the need to adapt to specific patient groups, such as pregnant women, and by the emergence of drug-resistant strains of Mycobacterium tuberculosis. Early detection and treatment are crucial for the prognosis of those affected.