The medical team in the internal medicine department hypothesized that it was leptospirosis.
Treatment and clinical course
Initial therapy:
- fasting and intravenous hydration;
- antibiotics: ampicillin/sulbactam 3 g x 4/day.
- potassium supplementation and platelet transfusion.
After a few hours, the patient was confused and disoriented. A brain CT scan excluded events acute, particularly hemorrhage.
The patient developed hyperpyrexia, hypotension, and acute pulmonary edema. ECG revealed atrial fibrillation with a ventricular rate of 160 bpm. Following transfer to the intensive care unit, she was successfully treated with parenteral antibiotics and intensive support.
Serology confirmed Leptospira infection.
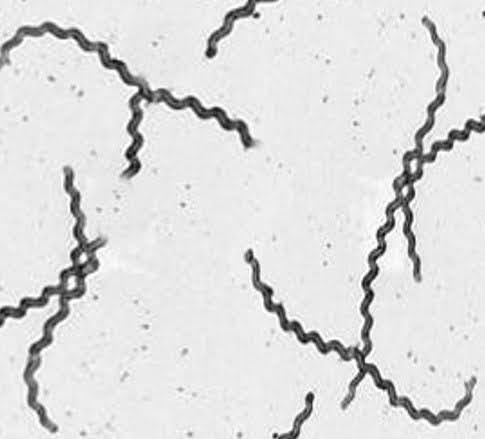
Leptospirosis, Dark-Field Microscopy. The characteristic spiral shape of this bacteria is demonstrated in the image. Contributed by S Bhimji, MD (Copyright © 2025, StatPearls Publishing LLC)
Update on Leptospirosis
Leptospirosis is an infectious disorder of animals and humans and is the most common zoonotic infection in the world. This infection is easily transmitted from infected animals through their urine, either directly or through infected soil or water. Leptospirosis can cause a self-limiting influenza-like illness or a much more serious disease. This condition is known as Weil disease, and it can progress to multiorgan failure with the potential for death.
The classic presentation of Weil's Syndrome, also called jaundiced Leptospirosis, includes jaundice, hemorrhagic diathesis, acute renal failure, and respiratory distress; it can also affect the heart, central nervous system, and muscles. The mortality rate correlates with the presence of altered mental status, acute renal failure, hypotension, and arrhythmias. Clinical manifestations are secondary to vasculitis (interstitial nephritis, hepatic centrolobular necrosis, alveolar hemorrhages, muscle necrosis, edema from increased capillary permeability).
While most Leptospira infections are asymptomatic or paucisymptomatic in humans, in a small percentage of cases they can result in severe infections and potentially fatal complications. Diagnosis is based on serology and PCR testing, as highlighted in this case. Early antibiotic therapy, combined with careful monitoring, is crucial to reducing mortality.
Conclusions
This case highlights the importance of considering rare infectious diagnoses, such as leptospirosis, in suggestive clinical contexts. Distinctive features like dehydration and oral cavity petechiae can be critical in directing the diagnostic suspicion. Timely management of complications and precise microbiological diagnostics are essential for ensuring a favorable outcome.