Considering the persistence of fever, recent splenomegaly, pancytopenia, and lack of response to empirical therapies, which of the following differential diagnoses is the most likely?
- Infective endocarditis
- Chronic lymphocytic leukemia
- Visceral Leishmaniasis
- Non-Hodgkin lymphoma
- Miliary tuberculosis
Diagnostic process discussion
The new finding of splenomegaly on physical examination and abdominal CT guided subsequent diagnostic steps. Given the correlation with the clinical picture and laboratory tests, particularly the bilineage cytopenia (anemia and leukopenia with neutropenia), it was hypothesized that splenic hyperplasia might be related to systemic infections. Oncological-hematological infiltrative forms and conditions with altered immune regulation such as SLE and Felty's syndrome were excluded due to lack of diagnostic criteria.
The degree of cytopenia did not correlate with the splenomegaly, which, although present, was mild. This led to the consideration of a condition directly responsible for cytopenia, as seen in some infections like zoonoses.
A hematology consult was requested, recommending a bone marrow aspirate and culture to clarify the etiology of the fever. On March 22, 2024, the patient underwent bone marrow aspiration for cytomorphology, flow cytometry, marrow culture, and zoonotic agent search. The examination revealed the widespread presence of Leishmania intracellularly and extracellularly; a finding compatible with Leishmaniasis.
The patient was thus diagnosed with visceral Leishmaniasis. In this patient, the visceral manifestation, characterized by splenomegaly and cytopenia due to marrow involvement, was exacerbated by the immunosuppression caused by chronic steroid therapy for his autoimmune hemolytic anemia.
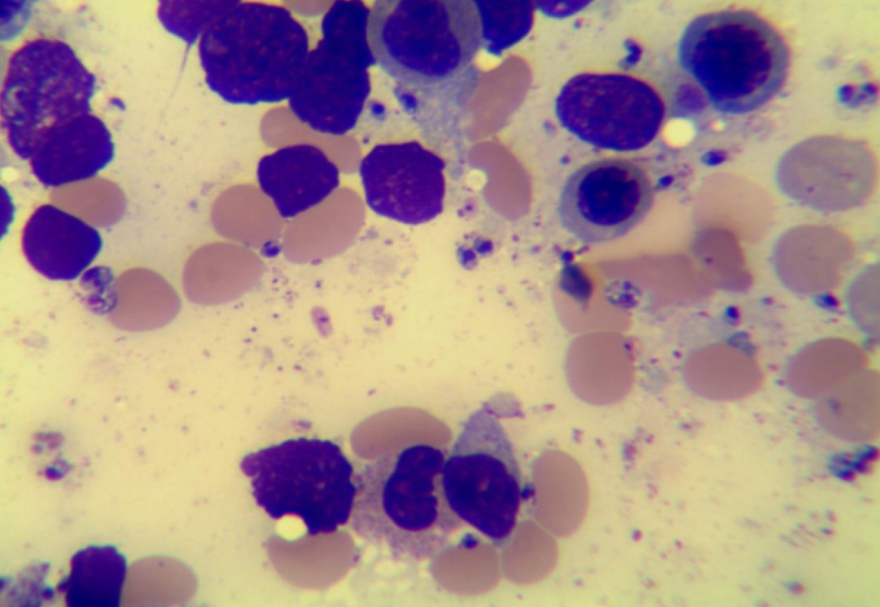
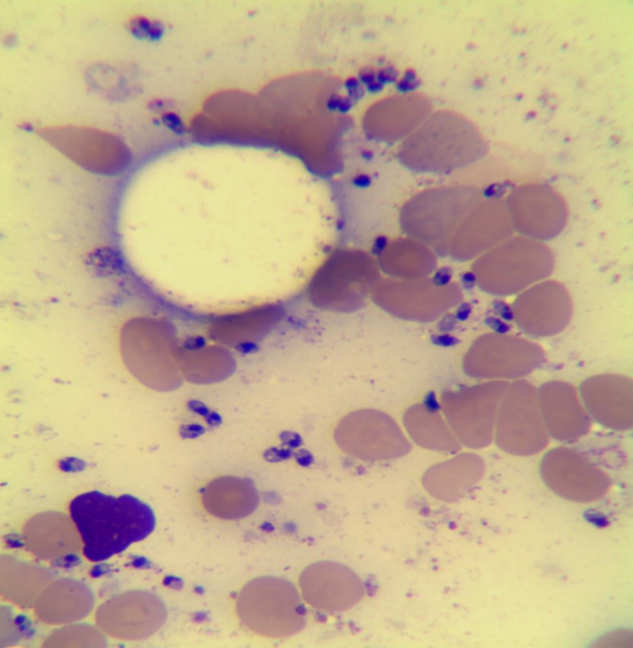
Bone marrow exam - The overall morphological pattern depicts a hyperplastic hematopoietic marrow with evidence of parasitic infection compatible with Leishmania.
The patient was treated with AmBisome (Liposomal Amphotericin B) 250 mg/day for 5 days. After therapy, the patient showed progressive improvement in general clinical condition, resolution of fever, and improvement in laboratory tests, until normalization of CBC values and liver cytolysis indices.
The patient was discharged on March 29.
Visceral Leishmaniasis
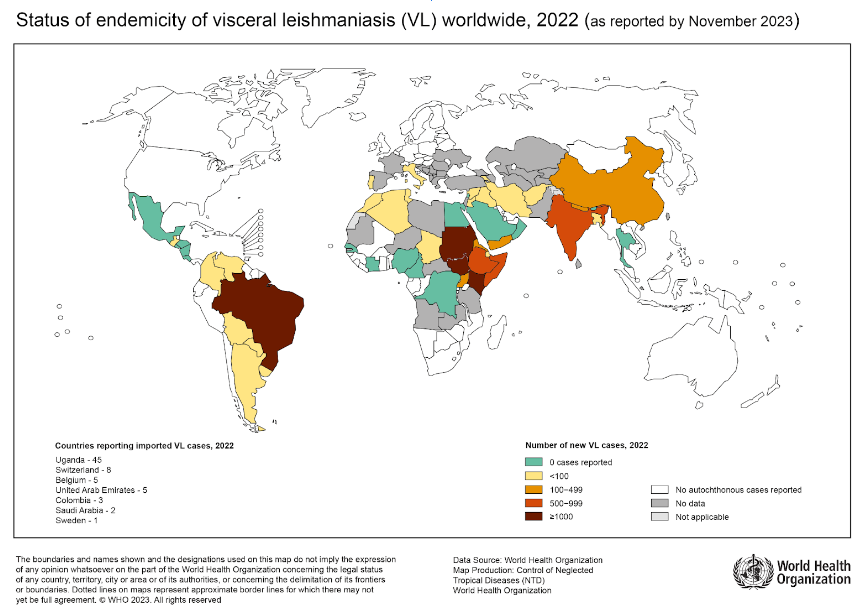
Leishmaniasis is a parasitic disease caused by infection with Leishmania parasites, which are spread by the bite of infected sand flies. The infection is endemic in 90 countries, tropical and subtropical and in Southern Europe, particularly in the Mediterranean basin. Transmission is usually by bite of haematophagous females of some sandfly species of the genera Phlebotomus (Europe, Asia and Africa) and Lutzomyia (Americas).
Dogs constitute the main reservoir of the parasite. Other domestic (e.g., cat, horse, and cattle) and wild species (e.g., fox and rat) may rarely manifest the disease but do not appear to serve as reservoirs.
There are several clinical manifestations: the cutaneous form, the mucocutaneous form and the visceral form. The cutaneous and mucocutaneous form can be considered manifestations with a benign course, while the visceral form has more severe systemic manifestations.
The visceral form courses in most cases as asymptomatic; risk factors for infection include hematologic malignancies, childhood age, transplantation, HIV infection, and immunosuppressive treatment.
The risk of manifestation of visceral Leishmaniasis after infection depends on several factors, the most significant of which is immunocompetence. This is why visceral Leishmaniasis is associated with immunosuppressive conditions.
Once infected, Leishmania replicates in the endothelial reticular system; a very high parasite load accumulates in the spleen, liver, and bone marrow.
Severe anemia may then occur due to bone marrow suppression, hemolysis, and splenic sequestration, which is associated with neutropenia and thrombocytopenia.
The infection has an incubation period of 2 to 6 months, and the onset of the disease, is almost never acute, but presents rather insidiously and subacutely, with nonspecific symptomatology characterized by fever, general malaise, asthenia with a worsening course, weight loss, anemia; splenomegaly and night sweats are sometimes present.
As the disease progresses, pancytopenia is observed with hemorrhagic complications, secondary bacterial infections, as well as cachexia and organ dysfunction. Without treatment, the mortality rate when the disease becomes manifest is over 90%.
Supportive therapy aimed at maintaining nutritional status, managing anemia, bleeding complications, and secondary infections. Liposomal amphotericin B is the most effective drug with a superior safety profile, lacking the toxic effects of the standard form (high risk of renal toxicity).
Visceral Leishmaniasis is a rare but possible condition, especially in endemic regions like Southern Italy. Leishmaniasis is classified as a neglected tropical disease by the World Health Organisation. However, an estimated 700,000 to 1 million new cases occur each year. These numbers may increase due to climate change. Increasing temperatures in temperate regions could in the future attract sand flies, which would then find new habitats.
Further information: Current WHO information on leishmaniasis