IBD and hormone therapies for cancer
The conclusions were reached by Jordan Axelrad and colleagues in a retrospective multi-center study for the New York Crohn's and Colitis Organization (NYCOO).
Hormone treatment for breast or prostate cancer may trigger IBD relapses
The conclusions were reached by Jordan Axelrad and colleagues in a retrospective multi-center study for the New York Crohn's and Colitis Organization (NYCOO) involving 447 IBD patients from five NYCOO-linked treatment centers.
In the study, 44% of patients suffered from Crohn's disease (CD), 53% from ulcerative colitis (UC) and 3% from non-classified IBD. 400 (90%) patients were at rest with their IBD at the start of cancer therapy, 47 (10%) were in an IBD relapse. 112 (28%) of patients with non-active IBD experienced a relapse of their bowel disease during cancer treatment. Both steroids (hazard ratio [HR]; 1.79; 95% confidence interval [CI] 1.18 - 2.71), immunomodulators (HR: 2.22; 95% CI 1.01 - 3.55) and biologics (HR: 1.95; 95% CI 1.01 - 5.36) were found to be associated with IBD relapses in IBD therapy (see Table 1), but not 5-ASA.
On the part of cancer treatment, both hormone monotherapy (HR: 2.00; 95% CI 1.21 - 3.29) and combination treatments of cytotoxic and hormone therapy (HR: 1.86, 95% CI 1.01 - 3.43) showed an increased risk of IBD relapses. 34 (8%) patients received exclusively cytotoxic chemotherapy. Of these, 75% remained in remission of their IBD even after 250 months. Of the 47 patients with active IBD at the onset of cancer treatment, 14 (30%) achieved remission, although no significantly responsible factor could be identified.
Hormone doses influence IBD disease activity
The aim of the study, which covered patients from 1997 to 2018, was to check whether IBD patients under hormone therapy had an increased risk of developing IBD relapses. The background to this question is the influence of sex hormones on the development of IBD, which has been significantly demonstrated in various contexts, such as cases of women under oral contraception.2 Postmenopausal hormone replacement therapy is also associated with an increased risk of UC.3 In addition, a summary evaluation of population-based studies has revealed evidence of the importance of sex hormones for the pathogenesis of IBD.4 Finally, IBD patients show a dependence of their disease progression and symptom severity on hormonal contraception and cyclic hormone fluctuations.5,6
Loss of estrogen-mediated immune protection and hormone-dependent dysbiosis?
Animal experiments have provided concrete evidence on the pathomechanism behind the influence of sex hormones, especially estrogen, on the development of IBD. Thus, estrogen is able to influence the intestinal permeability of the mucosal barrier and homeostasis, can impair the immune defence in the intestine and change the microbiome.7 Accordingly, the authors of the current study are not surprised by their results, although they explicitly point to weaknesses of their investigation, such as its retrospective character.
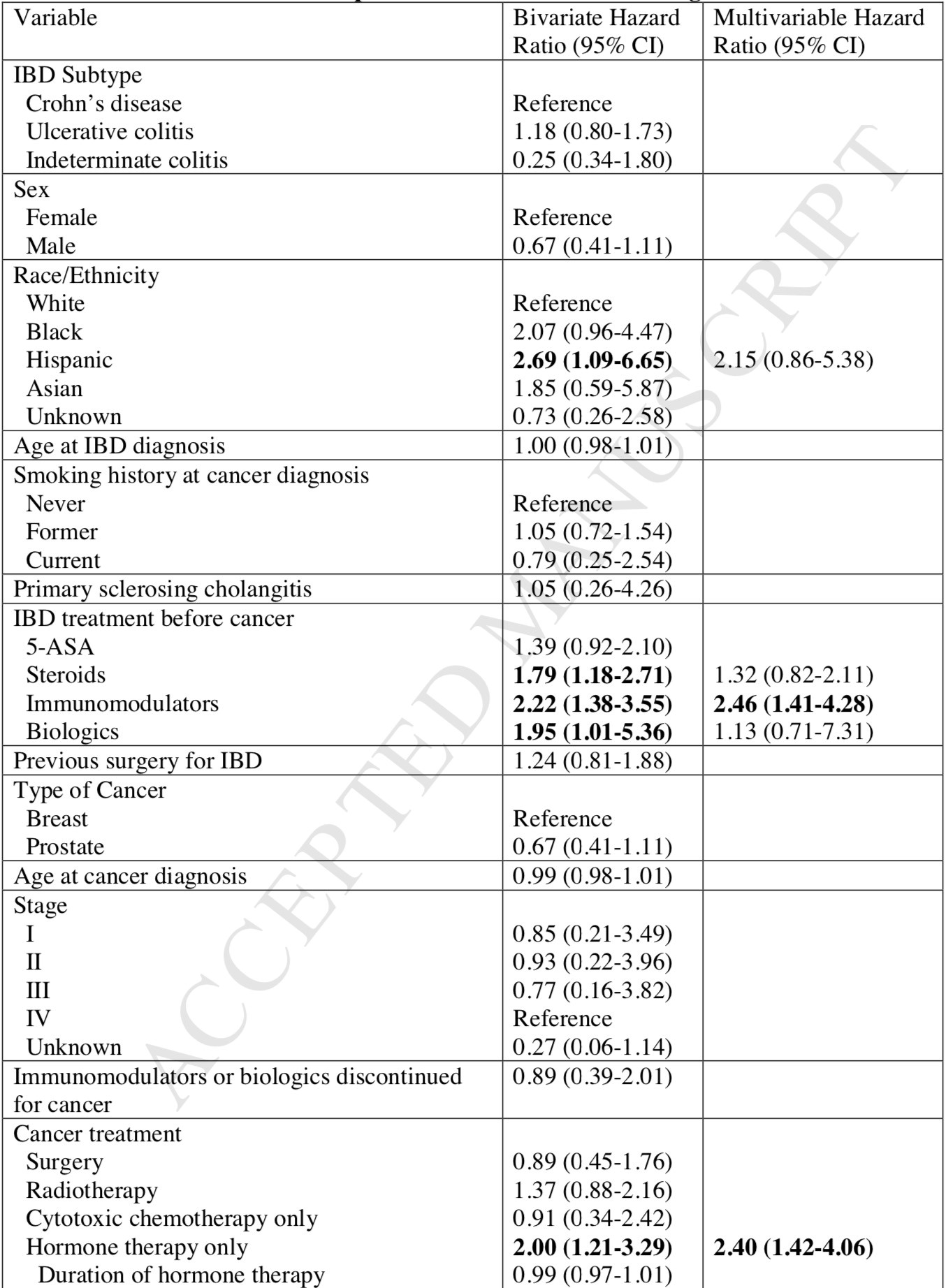

Table 1: Risk for IBD relapses in non-active IBD at the time of cancer diagnosis1
References:
1. Axelrad JE, et al. Hormone Therapy for Cancer is a Risk Factor for Relapse of Inflammatory Bowel Diseases, Clinical Gastroenterology and Hepatology. 2019. Epub ahead of print. https://doi.org/10.1016/j.cgh.2019.06.042.
2. Ortizo R, et al. Exposure to oral contraceptives increases the risk for development of inflammatory bowel disease: a meta-analysis of case-controlled and cohort studies. Eur. J. Gastroenterol. Hepatol. 2017; 29: 1064–1070. https://www.ncbi.nlm.nih.gov/pubmed/28542115.
3. Khalili H, et al. Hormone therapy increases risk of ulcerative colitis but not Crohn’s disease. Gastroenterology 2012; 143: 1199–1206. https://www.ncbi.nlm.nih.gov/pubmed/22841783.
4. Shah SC, et al. Sex-Based Differences in Incidence of Inflammatory Bowel Diseases-Pooled Analysis of Population-Based Studies From Western Countries. Gastroenterology 2018; 155: 1079–1089.e3. https://www.ncbi.nlm.nih.gov/pubmed/29958857.
5. Gawron LM, Goldberger A, Gawron AJ, et al. The impact of hormonal contraception on disease-related cyclical symptoms in women with inflammatory bowel diseases. Inflamm. Bowel Dis. 2014;20:1729–1733. https://www.ncbi.nlm.nih.gov/pubmed/25105949.
6. Rolston VS, Boroujerdi L, Long MD, et al. The Influence of Hormonal Fluctuation on Inflammatory Bowel Disease Symptom Severity-A Cross-Sectional Cohort Study. Inflamm. Bowel Dis. 2018;24:387–393. https://www.ncbi.nlm.nih.gov/pubmed/29361085.
7. Org E, et al. Sex differences and hormonal effects on gut microbiota composition in mice. Gut Microbes 2016; 7: 313–322. https://www.ncbi.nlm.nih.gov/pubmed/27355107.