Microangiopathy and long COVID
An early sign of cerebral microangiopathy can be absent-mindedness that begins in adulthood. In addition, a silent stroke can also lead to concentration problems.
What role does the vascular system play in Long COVID?
Since the emergence of SARS-CoV-2, another cause of distraction and concentration problems has been added to cerebral microangiopathy and silent stroke. The memory and concentration disorders that occur in Long COVID are also called "brain fog". The pathomechanism behind Long COVID is not yet fully understood. Scientific research in ophthalmology suggests a vascular pathomechanism for Long COVID. For example, hypoperfusion of the choroid of the eye has been observed in patients with Long COVID. By means of imaging techniques, haemangioma-like lesions could be detected in the area of the choroid of the affected patients. The vessels had been hyperpermeable in some areas. From an embryogenetic point of view, the eye is an outpouching of the brain. The extent to which these observations on the ocular vessels can be transferred to the brain still needs to be examined. An important aspect that speaks in favour of this is the treatment success with BC 007 in patients with long COVID. The target structure of the BC 007 drug includes autoantibodies directed against the endothelin A receptor and also against alpha1-adrenergic, beta1- and beta2-adrenergic receptors.3,4
SARS-CoV-2 and thrombosis
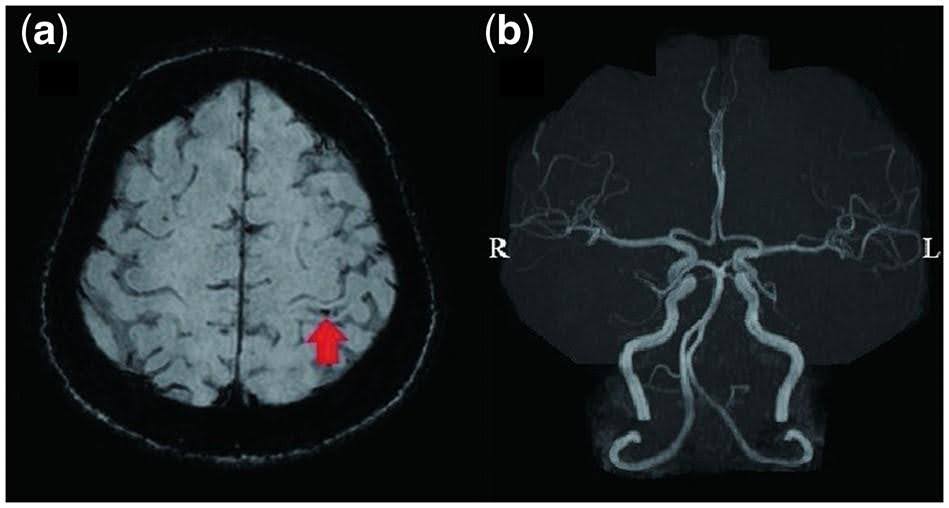
Vascular changes appear to occur in various forms in some patients with SARS-CoV-2 infection. In addition to hypoperfusion and hyperpermeability of smaller vessels, thrombosis may also occur. Macrovascular and also microvascular thrombosis can occur in the course of SARS-CoV-2 infection. Case reports have described extensive microvascular thrombosis. Thrombotic microangiopathy could be a contributory cause of the thrombotic and multi-organ complications of COVID-19.5 An interesting case report on this topic was published on 15 June this year. A 56-year-old female patient with severe COVID-19 disease and cerebral microangiopathy had no obvious abnormalities on MRI (see Figure 1). This seemed extremely unusual to Ymoto W. According to Imoto W., such a case may be a microangiopathy triggered by COVID-19.5
COVID-19 associated encephalopathy
To date, we know little about the symptomatology of COVID-19 associated cerebral microangiopathy or encephalopathy. According to case reports, COVID-19-associated encephalopathy can present with a wide spectrum of symptoms and clinical manifestations. Patients with COVID-19-associated encephalopathy may experience the following:
- Dizziness
- Headache
- Anxiety
- Depression
- Strokes
- Epileptic seizures
- Guillain-Barre syndrome (GBS)
- Demyelinating diseases5
Currently, many researchers still have questions about the cause of COVID-19 associated sequelae. We know that severe COVID-19 disease can manifest as multi-organ dysfunction. The most common organ involved is the lung. There is evidence that an excessive immune response is the driving factor. Organ damage can occur as a result of unchecked complement activation and a cytokine storm. Furthermore, it is known that patients with severe COVID-19 disease may have hypercoagulability and thus a tendency to thrombosis. In addition to macrovascular, microvascular thrombi also play a role in multi-organ failure. Thrombotic microangiopathy can also occur in the CNS area.6
The vascular system of the CNS can be studied in the eye
The influence of a SARS-CoV-2 infection on the vascular system of the human eye has been investigated in various studies. These include preparatory studies of the ReCOVer study at the University Hospital Erlangen (Germany). The eye as an extension of the brain offers us the possibility to investigate the effects of a SARS-CoV-2 infection non-invasively, e.g. by means of OCT. Recently, a study on COVID-19-associated choroidopathy was published. In this prospective study, patients who had to be hospitalised due to a severe COVID infection were examined using indocyanine green angiography (ICGA) and OCT diagnostics. These two methods from ophthalmology are used to examine the retina and the choroid. The choroid is also called the choroid. The name comes from the strong vascularisation of the choroid. It consists of several layers with larger arteries and veins and fine fenestrated capillaries. Vascular anomalies were detected in all patients examined. Lesions of both retinal and choroidal vessels were noted.7
It is important to investigate how these COVID-19-associated vascular anomalies or microangiopathies and thromboses are related to the cerebral symptom complexes that we may encounter in a post-COVID setting.
1. Absentmindedness points to earlier warning signs of silent strokes among people at risk. ScienceDaily Available at: https://www.sciencedaily.com/releases/2019/02/190206091417.htm. (Accessed: 20th March 2019).
2. Dey A. K. et al. (2019). Cognitive heterogeneity among community-dwelling older adults with cerebral small vessel disease. Neurobiology of Aging 77, 183–193.
4. https://ichgcp.net/de/clinical-trials-registry/NCT04192214
5. Imoto W. et al. (2022). Long COVID with intracranial microangiopathy. QJM. 2022 Aug 13;115(8):539.
6. Tiwari NR, Phatak S, Sharma VR, Agarwal SK. COVID-19 and thrombotic microangiopathies. Thromb Res. 2021 Jun;202:191-198.
7. Abdelmassih Y. et al. (2021). COVID-19 associated choroidopathy. J Clin Med 2021;10:4686.