Consultations: An end to delays thanks to AI?
Streamlining consultations thanks to a virtual assistant. A real cerebral and technical prosthesis that helps to manage physicians' time. Make way for new technologies and AI!
Joris Galland is a specialist in internal medicine. After working at the Lariboisière Hospital (AP-HP), he joined the Bourg-en-Bresse Hospital. Passionate about new technologies, he aims to explain the issues at hand in our blog.
The title is a bit provocative, of course... but as a physician I am often embarrassed to have to keep patients waiting during my consultations. But in fact, why can a consultation cause delay? First of all, let's remember that a consultation generally takes place in three stages: The questioning of the patient, the physical examination and the writing of prescriptions. A consultation is intended to last a limited time. In internal medicine, I can theoretically devote 40 minutes to a patient who consults me for the first time and 15-20 minutes for subsequent consultations.
I'm not telling you anything new, the consultations follow one another and are not the same. Not to mention the so-called "unscheduled" ones where we have to see a patient urgently, between two consultations. The result is delay and stress... A consultation schedule is a bet on the future based on a theoretical average duration per patient. As time is incompressible, it happens - I don't think I'm being too forward - that we overflow. In my opinion, there are certain moments in a consultation that cannot be cut short: The moment when we listen to the patient's complaints and the moment when we examine him. For the rest, it is a simple race against the clock. And in this race, AI enters the track.
What health professional has not dreamed of this? To streamline their consultations thanks to a virtual assistant, a real cerebral and technical prosthesis that helps them manage their time. Make way for new technologies and AI!
Save time before the consultation
Without entering the realm of telemedicine or tele-expertise, easy-to-use applications allow patients to collect their health data before or between consultations.
These applications offer the patient:
- Questionnaires to assess their state of health
- An interface for importing biological, radiological or "quantified self" data (collected via connected objects)
Let's take the example of oncology. Cancer treatment requires multiple medical consultations that result in exhausting trips home and back to the hospital for the patient. With the Chimio1 application, the patient can assess the symptoms caused by their treatment at home on a daily basis. Depending on their number, severity, frequency and duration and the impact on daily life, an algorithm classifies these symptoms into four levels of urgency. Depending on the severity of the alert, a teletransmission is carried out in order to prepare a graduated response and to coordinate care between the city and the hospital.
The aim is to reduce unscheduled consultations and hospitalisations by anticipating and managing urgent situations in real time. But it also allows sufficient time for the consultation because the physician already knows whether the patient is in good general condition - in which case the consultation will be quick - or whether he or she is relapsing, which means that the consultation will be long and may lead to hospitalisation.
These pre-consultation health applications allow for closer monitoring of patients and more relevant collection of information on the evolution of the disease. Above all, they use algorithms that predict the risk of an unfavourable outcome. This is the case with the Moovcare application: Its algorithm detects lung cancer relapses based on a simple questionnaire that patients fill in once a week.
Before the consultation, these applications can therefore prevent the patient from consulting in a hurry, by better anticipating their needs. But they can also systematically prevent them from coming for a follow-up consultation, when they could only consult when necessary - the AI would then be responsible for scheduling the consultations. Personally, I still resent making patients come for a consultation every three months to comply with the recommendations, even if the evolution of their health is favourable and would require a consultation every six months. It remains to democratise these AIs for the monitoring of other chronic diseases, and to trust them to decide on the appropriate follow-up according to health questionnaires and biological results. Personally, such applications could free up my consultation slots, and avoid my new patients having to wait three months for a first consultation.
Second round: During the consultation
The most important part of the consultation is the taking of vitals. A ritual that is repeated for each patient and takes 2 to 3 minutes. This may not seem like much, but it represents between 10 and 20% of the consultation time. AI can help us to shorten this time, which I would prefer to devote to listening to the patient and establishing a more empathetic relationship. The Binah.ai2 solution - and the French solution Quantiq, which is currently being tested - allows vital signs to be taken in a few seconds, with a simple smartphone camera pointed at the patient's face, more precisely at the upper cheek. The physical data from the video is then analysed by the AI.
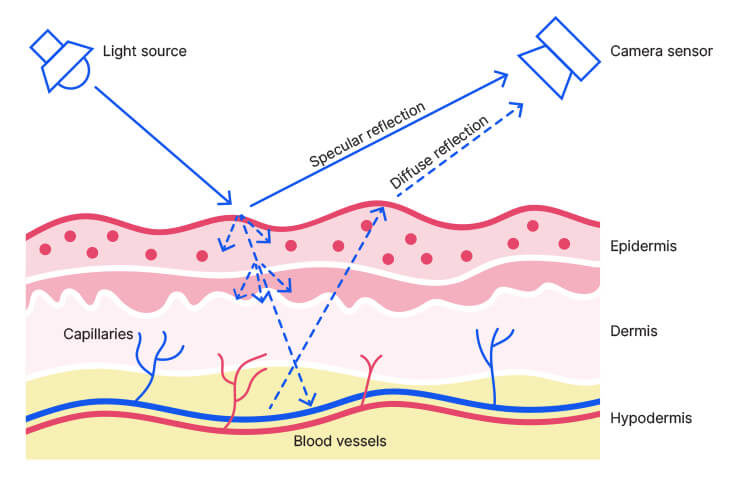
Magic? No, just a sharp point of technology... and especially of physics: Binah.ai measures the changes in the reflection of red, green and blue light on the skin, quantifying the contrast between "specular" and "diffuse" reflection. The process is called "remote photoplethysmographic imaging" and also works by placing the user's finger on the smartphone camera. Better still, this tool works in teleconsultation and could even make it possible to "monitor" patients in intensive care, without the need for scopes and sensors.
Credit: Binah.ai
End of the consultation. The time has come for a "pet peeve" of many physicians: Writing prescriptions. Not to mention the famous "prescription renewal" consultations, so time-consuming when the patient comes with a prescription as long as his arm. It's hard to sort out, hard to know all the interactions, and it's hard to believe that you have to copy everything!
Fortunately, AI is here to help us. The French applications Synapse3 and Posos4 can scan the prescription via a smartphone camera or detect the drugs on the prescription in order to analyse them and even display dangerous drug interactions or contraindications. To top it all off, Posos even offers alternative substances! From my point of view as a physician, this is a small revolution.
In the short term, these apps will make it possible to communicate directly with the computerised patient file, for example to link the adaptation of the dosage with the patient's renal and hepatic function or allergies. This is a godsend, given that each year in France, these errors are responsible for 10,000 to 20,000 serious adverse events and could be the cause of 1,000 deaths. An unacceptable human cost, a non-negligible financial cost.
From stethoscope to smartphone
We can see from these few examples (there are many others!) that AI will be able to relieve the physician of a certain mental - and administrative! - burden to concentrate on the patient. This is the idea that the National Council of the Order of Physicians defended in its white paper on AI.5
Crédits : binah.ai
The medical consultation is a moment of meeting and exchange in a limited time. There is no room for parasitic tasks. AI can assist us at all stages of our consultations: preparation, data synthesis, clinical examination and therapeutic decision making. In the short term, this complementarity between humans and AI will make the patient's pathway more fluid and improve the physician's performance and speed - while preserving the quality and safety of care.
References:
1. CHIMIO application
2. Binah.ai - Vital Signs Monitoring for Everyone, Everywhere
3. Synapse application
4. Posos application
5. Cnom - Médecins et patients dans le monde des data, des algorithmes et de l’intelligence artificielle