Escitalopram and psilocybin in healthy subjects
The results of a study in healthy volunteers presented by Dr. Anna Becker suggest that SSRIs should not be discontinued prior to psilocybin treatment.
Effects of pretreatment with SSRIs on subjective response to psilocybin in healthy subjects
The results of a study in healthy volunteers presented by Dr. Anna Becker suggest that SSRIs should not be discontinued prior to psilocybin treatment. After two weeks of pretreatment with escitalopram, some adverse effects of psilocybin were also reduced.
Psilocybin (the active ingredient in so-called 'magic mushrooms') is a classic serotonergic hallucinogen that acts on the serotonin 5-HT2A receptor. It is a precursor that is activated to psilocin in the body. Its effects are mainly mediated by partial agonism at the 5-HT2A serotonin receptor. Psilocybin is used for recreational purposes and in psychiatric research. The effects of mushrooms, which grow in the wild and have been used since ancient times as healing remedies and intoxicating substances, range from euphoric and hilarious to highly hallucinogenic and psychedelic, altering the perception of time and space, distorting the sensation of one's surroundings. Psilocybin is studied as a treatment for a variety of psychiatric disorders, including mood and anxiety disorders.
The first-line therapy for patients with mood and anxiety disorders are now selective serotonin reuptake inhibitors (SSRl), which acutely increase serotonin (5-HT) levels in brain synapses. However, mood elevating effects generally occur after several weeks of repeated daily treatment and are probably associated with adaptive changes in the brain. Escitalopram, a drug often used to treat depressive episodes, acts as an inhibitor of the serotonin transporter (SERT). The link between this mechanism and its positive effects on mood remains to be established. Several studies suggest a possible down regulation of postsynaptic serotonin (5-HT) receptors such as the 5-HT2A receptor.
The aim of the study conducted by researchers at the University of Basel, coordinated by Prof. Matthias Liechti, was to assess whether inhibition of the SERT transporter reduced the expression of the gene encoding for the 5-HT2A receptor and the response to psilocybin. For phase two studies and compassionate use programmes using psilocybin, it will be important to know whether patients should stop their SSRI treatment prior to psilocybin administration. The results of the study were presented by Dr. Anna Becker at the INSIGHT 2021 conference.
Participants took escitalopram (10 mg in the first and 20 mg in the second week) or placebo for 14 days. Then a single dose of psilocybin (25 mg) was administered. The primary endpoint of the study was subjective effects on consciousness (measured with the 5D-ASC scale). Secondary endpoints included further psychological measurements, plasma concentrations of psilocybin and escitalopram, gene expression of the HTR receptor, as well as some safety measures (effects on the autonomic nervous system, ECG).
Dr. Becker at INSIGHT 2021 conference
(Photo: Samuli Kangaslampi)
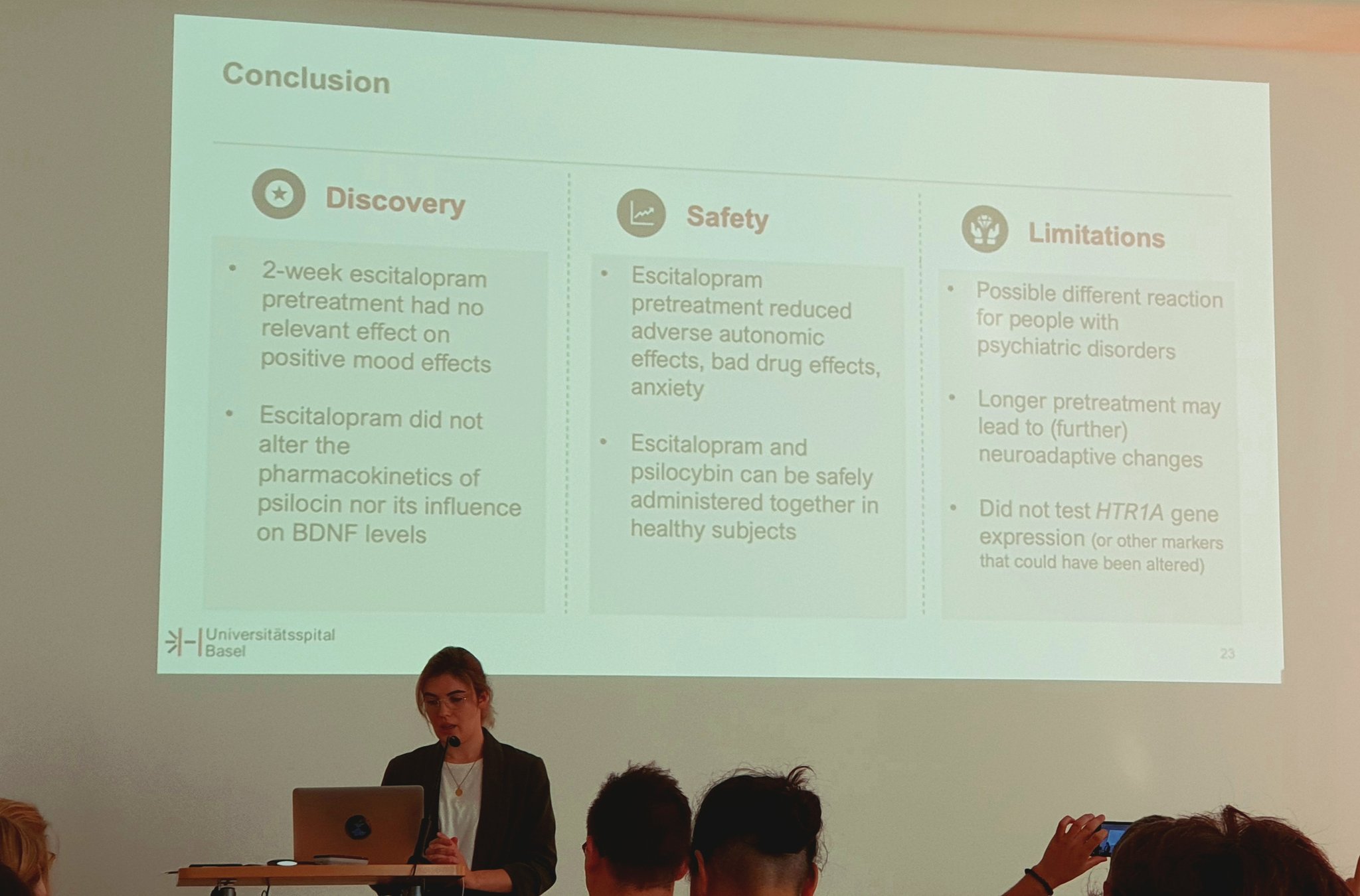
The research found that 2 weeks of pretreatment with escitalopram had no significant effect on positive mood effects. Escitalopram did not alter the pharmacokinetics of psilocin or its influence on BDNF (Brain-derived neurotrophic factor) levels. Furthermore, pretreatment with escitalopram reduced the adverse effects of psilocybin. Thus, in healthy subjects, escitalopram and psilocybin can be safely administered together.
Dr. Becker believes that further research is needed to overcome the limitations of this study. There may be a different reaction in people with psychiatric disorders. Furthermore, a longer pre-treatment could lead to (further) neuroadaptive changes. Another limitation of this study is that the expression level of the HTR1A gene (or other markers that might have been altered) was not measured.
Reference:
Becker A, Effects of Serotonin Reuptake Inhibitor (SSRI) Pretreatment on the Subjective Response to Psilocybin in Healthy Subjects, Insight 2021